insights
Functional Medicine Matrix: Organizing Clinical Imbalances

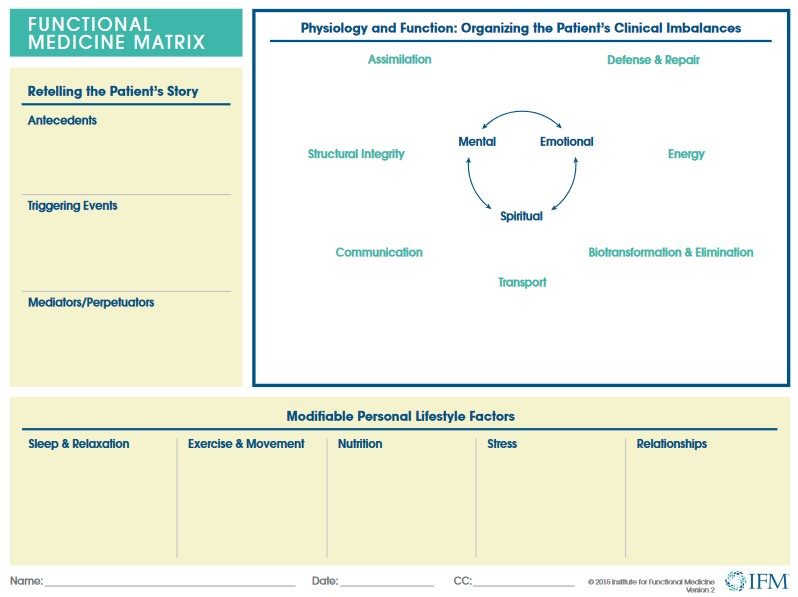
Functional medicine recognizes that illness does not occur in isolation, and the tools in IFM’s Toolkit, such as the matrix, help clinicians examine the body systems, symptoms, and risk factors associated with their patient’s health conditions. Specifically, the matrix provides an outline for the clinician to organize a patient’s clinical imbalances in the following biological systems, called nodes: defense and repair, energy, biotransformation and elimination, transport, communication, structural integrity, and assimilation.
The left section of the matrix is useful in retelling the patient’s story by tracking antecedents, triggering events, and mediators/perpetuators. The bottom of the matrix details lifestyle factors like sleep and relaxation, exercise and movement, nutrition and hydration, stress and resilience, and relationships and support networks.
As a whole, the functional medicine matrix assists the clinician in organizing and prioritizing each patient’s health issues as elicited by a thorough personal, family, social, and medical history. The matrix is a tool for organizing what may seem to be disparate issues into a complete story to help the clinician gain a comprehensive perspective of the patient and subsequently facilitate discussion of complex, chronic disease.
Download the Functional Medicine Matrix
IFM members gain access to the matrix in the IFM Toolkit, which is an exclusive benefit of IFM membership. Non-IFM members may receive temporary toolkit access for the duration of selected courses, including Applying Functional Medicine in Clinical Practice (AFMCP) and the Advanced Practice Modules (APMs).
As a member, how do I access the IFM Toolkit?
- Log in to the IFM website and select “My Toolkit.”
- Note: If you do not see the mentioned links, check your membership status from the “My Certification & Membership” tab.
Related Articles
The Role of Empathy and Storytelling in Functional Medicine
Diet, Nutrition, and Lifestyle Journal Helps Patients Track Daily Choices