insights
Personalizing Nutritional Interventions

Read Time: 3 Minutes
With the rising prevalence of chronic disease,1 nutrition-based interventions are fundamental components of many therapeutic strategies for disease treatment and prevention.2 A variety of factors shape personalized nutritional therapies. For example, a patient’s specific chronic disease, underlying nutrient deficiency, or presentation of disease symptoms may direct a nutritional approach to include or exclude certain foods or require a clinician to create a tailored dietary plan to support certain body systems. An individual’s biochemical response to foods is also an important consideration, as millions of people are diagnosed with food allergies in the United States3 and some experience non-allergy food sensitivities that may trigger gastrointestinal (GI) symptoms4 or extraintestinal manifestations. Personalized nutrition interventions may also incorporate a patient’s health goals and motivations, cultural and personal preferences, genetic profile, and circadian rhythms, all to potentially enhance patient empowerment and treatment sustainability. Personalizing nutrition-based interventions, including therapeutic food plans, helps to create the most appropriate and effective wellness strategy for each individual patient.
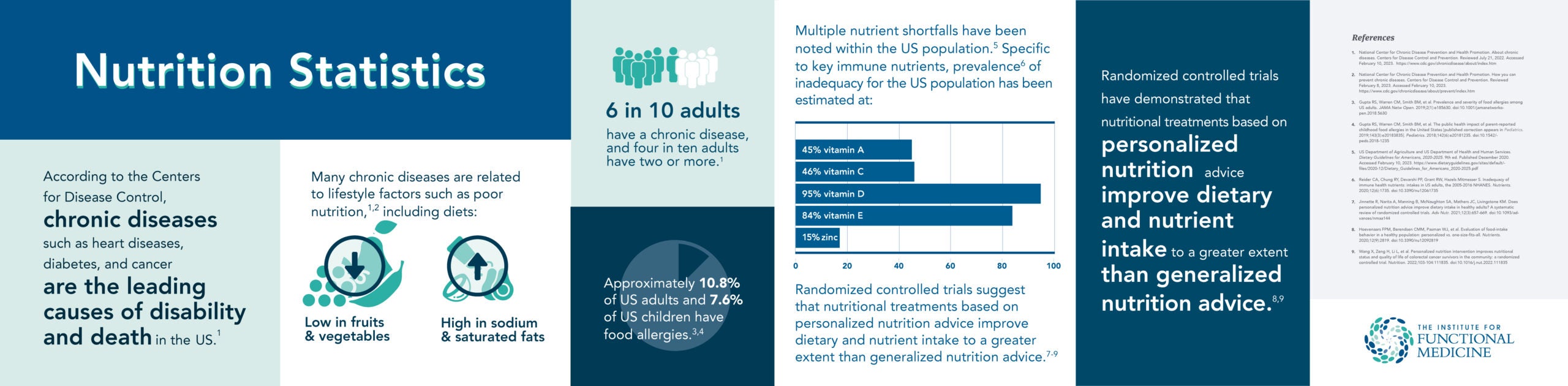
A nutritional treatment may fit one patient perfectly but require extensive modifications to meet another patient’s health needs. Personalized nutrition has been described as a health field and treatment approach that uses a patient’s individuality to inform nutrition strategies that help to prevent, manage, or treat disease and promote optimal health.5 A 2021 systematic review of 11 randomized controlled trials (RCTs) found that compared to generalized nutrition advice, personalized nutrition improved dietary intake in healthy adult populations.6 As an example, a 2021 RCT (n=1,270 adults; 46% had overweight/obesity) reported that following a six-month intervention period, personalized nutrition advice resulted in greater reductions of discretionary foods intake (foods high in fat, added sugars, and salt) compared to generalized nutrition advice.7 In addition, a 2022 RCT (n=56 colorectal cancer survivors) measured the nutrition status, dietary intake and quality of life among patients who followed personalized nutritional interventions versus those who received routine care.8 After six months, the intervention group had higher energy and protein intake and gained more weight than the routine care group. In addition, those in the intervention group had a significantly higher global health status and overall quality of life compared to controls.8
Increasing fiber consumption, prioritizing healthy fat intake, and avoiding trigger foods are just some nutritional factors that are associated with preventing, treating, or managing different chronic diseases. Plant-based diets have been linked to a lower risk of developing cardiovascular disease;9 the Dietary Approaches to Stop Hypertension (DASH) diet has been shown to lower blood pressure in adults with and without hypertension;10 the low-FODMAP diet has been shown to reduce symptom severity in patients with irritable bowel syndrome (IBS);4 and the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet has been associated with less cognitive decline, reduced risk of dementia, and reduced severity of headaches.11,12 Using the components of personalized nutrition, these and other dietary approaches that have already shown effectiveness in the prevention or treatment of chronic disease can be tailored to meet each patient where they are in their health journey.
IFM’s suite of therapeutic food plans are all available for modification based on an individual’s health needs. Learn more about food plan personalization within the IFM framework and creating effective and sustainable nutrition-based strategies to promote health through the online course, Therapeutic Food Plans: A Component of Personalized Nutrition.
Related Articles
FOOD FIRST: DIETARY CHANGE IMPROVES OUTCOMES
Therapeutic Food Plans: A Component of Personalized Nutrition
Engaging Patients in Nutritional Therapy
References
- National Center for Chronic Disease Prevention and Health Promotion. About chronic diseases. Centers for Disease Control and Prevention. Reviewed July 21, 2022. Accessed March 6, 2023. https://www.cdc.gov/chronicdisease/about/index.htm
- National Center for Chronic Disease Prevention and Health Promotion. How you can prevent chronic diseases. Centers for Disease Control and Prevention. Reviewed February 8, 2023. Accessed March 6, 2023. https://www.cdc.gov/chronicdisease/about/prevent/index.htm
- Gupta RS, Warren CM, Smith BM, et al. Prevalence and severity of food allergies among US adults. JAMA Netw Open. 2019;2(1):e185630. doi:1001/jamanetworkopen.2018.5630
- Black CJ, Staudacher HM, Ford AC. Efficacy of a low FODMAP diet in irritable bowel syndrome: systematic review and network meta-analysis. Gut. 2022;71(6):1117-1126. doi:1136/gutjnl-2021-325214
- Bush CL, Blumberg JB, El-Sohemy A, et al. Toward the definition of personalized nutrition: a proposal by the American Nutrition Association. J Am Coll Nutr. 2020;39(1):5-15. doi:1080/07315724.2019.1685332
- Jinnette R, Narita A, Manning B, McNaughton SA, Mathers JC, Livingstone KM. Does personalized nutrition advice improve dietary intake in healthy adults? A systematic review of randomized controlled trials. Adv Nutr. 2021;12(3):657-669. doi:1093/advances/nmaa144
- Livingstone KM, Celis-Morales C, Navas-Carretero S, et al. Personalised nutrition advice reduces intake of discretionary foods and beverages: findings from the Food4Me randomised controlled trial. Int J Behav Nutr Phys Act. 2021;18(1):70. doi:1186/s12966-021-01136-5
- Wang X, Zeng H, Li L, et al. Personalized nutrition intervention improves nutritional status and quality of life of colorectal cancer survivors in the community: a randomized controlled trial. Nutrition. 2022;103-104:111835. doi:1016/j.nut.2022.111835
- Kim H, Caulfield LE, Garcia-Larsen V, Steffen LM, Coresh J, Rebholz CM. Plant-based diets are associated with a lower risk of incident cardiovascular disease, cardiovascular disease mortality, and all cause mortality in a general population of middle-aged adults. J Am Heart Assoc. 2019;8(16):e012865. doi:1161/JAHA.119.012865
- Filippou CD, Tsioufis CP, Thomopoulos CG, et al. Dietary Approaches to Stop Hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr. 2020;11(5):1150-1160. doi:1093/advances/nmaa041
- van den Brink AC, Brouwer-Brolsma EM, Berendsen AAM, van de Rest O. The Mediterranean, Dietary Approaches to Stop Hypertension (DASH), and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diets are associated with less cognitive decline and a lower risk of Alzheimer’s disease—a review. Adv Nutr. 2019;10(6):1040-1065. doi:1093/advances/nmz054
- Askarpour M, Yarizadeh H, Sheikhi A, Khorsha F, Mirzaei K. Associations between adherence to MIND diet and severity, duration and frequency of migraine headaches among migraine patients. BMC Res Notes. 2020;13(1):341. doi:1186/s13104-020-05181-4




