insights
Low-Level Lead Exposure & Implications for Human Health

Read Time: 6 Minutes
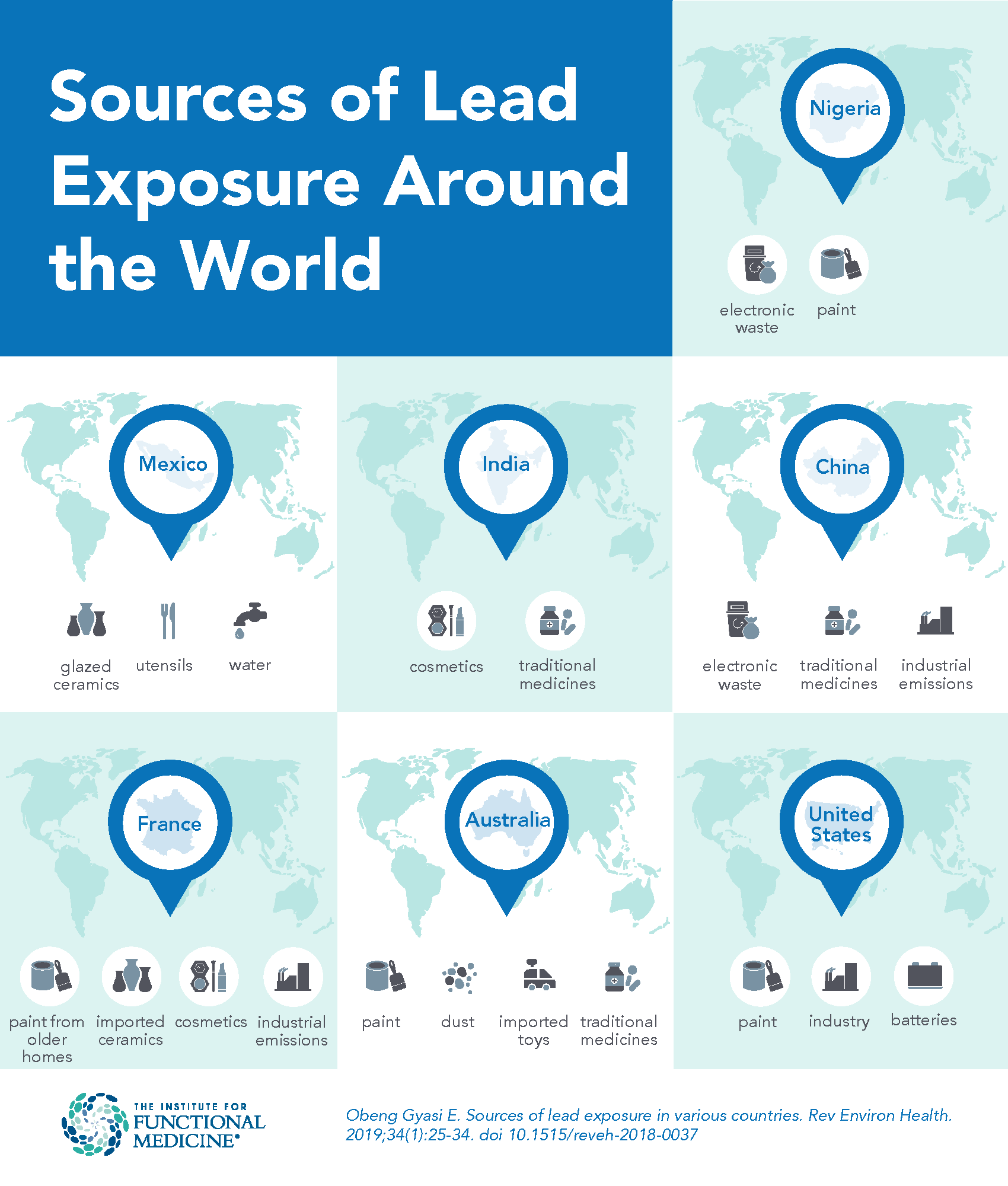
Lead is one of the most widely used metals in the world, and although it is toxic, it has been incorporated into many different products, including paints, cosmetics, fuels, and more, for its unique properties, such as a low melting point and resistance to corrosion. However, lead persists in the environment and cannot be metabolized in the human body.1 It can enter the body via a variety of routes; for example, particles from lead-based paint or housing renovation can adhere to food and be ingested, or industries that use lead in manufacturing can pollute the air and soil, exposing humans via the food chain.2
Global statistics from 2019 estimate that lead exposure accounted for nearly one million deaths and 21.7 million years of healthy life lost due to long-term health effects.3 Further, exposure to this heavy metal reportedly accounted for 30% of the global burden of idiopathic developmental intellectual disability, 4.6% of the global burden of cardiovascular disease, and 3% of the global burden of chronic kidney disease.3
Lead can be absorbed by the intestine and through the skin, and almost 90% of it binds to erythrocyte proteins.4 Once inside the human body, lead may travel to different tissues and organs, including the liver and kidneys, where it can cause oxidative damage to cells and tissues, including uncoupling the respiratory chain in mitochondria.4
A 2018 study provided the first published evidence that lead exposure results in DNA damage via promoting oxidative stress and promoter methylation of DNA repair genes in human lymphoblastoid TK6 cells.1 A 2021 systematic review and meta-analysis of 45 studies further indicated that chronic lead exposure is associated with DNA damage characterized by several components such as chromosomal aberrations and oxidative DNA damage.5
Lead Exposure and Cardiovascular Disease
A 2018 study published in The Lancet Public Health suggests that of the 2.3 million deaths every year in the United States, about 400,000 are attributable to lead exposure, of which 250,000 are from cardiovascular disease.6 This estimate is about 10 times larger than previous approximations.6 A 2019 US cross-sectional study showed that lead exposure affects cardiovascular markers in young and middle-aged adults (18-65 years), with higher exposure increasing with age and generally resulting in worse health outcomes.7 The study suggests that increasing levels of lead exposure may contribute to people being propelled toward various cardiovascular pathologies.7
While blood lead levels (BLLs) above 5 µg/dL in adults are considered elevated, sufficient evidence suggests that even BLLs <5 µg/dL are associated with decreased renal function and that BLLs <10 µg/dL are associated with increased blood pressure and hypertension.8 The mechanism by which lead induces hypertension may be related to oxidative stress, inflammation, alterations in the renin-angiotensin-aldosterone system, alteration of vasoactive and volume regulatory hormones, and nitric oxide dysregulation.7 Other conditions associated with lead exposure include:
- Cardiovascular disease due to telomere shortening and lipid disturbance.9
- Peripheral arterial disease, electrocardiographic abnormalities, and left-ventricular hypertrophy.6
- Kidney damage via oxidative stress and lipid peroxidation4 and chronic kidney disease reflected by decreased estimated glomerular filtration rate and increased proteinuria.10
- Respiratory, neurologic, digestive, and urinary diseases.11
Lead Exposure in Children
In children, there is no identified threshold or “safe” blood lead level below which no risk of poor developmental or intellectual function is expected.8 Young children are particularly vulnerable to lead poisoning because they absorb four to five times as much ingested lead as adults from a given source.3 In October 2021, the Centers for Disease Control and Prevention (CDC) updated the BLL value from 5 µg/dL to 3.5 µg/dL to identify those children with BLLs that are higher than most children’s levels.12 With the new measurement, the CDC estimates that 2.5% of US children aged one to five years have BLLs above 3.5 µg/dL.12
A 2019 cohort study was one of the longest and largest psychiatric follow-up studies involving children tested for lead exposure and followed 579 New Zealand children for more than 30 years.13 Researchers reported BLLs above the previous reference value for clinical attention (5 µg/dL) in 94% of the children, and childhood BLL was significantly associated with higher general psychopathology as well as internalizing and thought disorder symptoms into adulthood.13 Childhood BLL was also significantly associated with lower conscientiousness and agreeableness and higher neuroticism in adulthood.13
It is interesting to note that while thousands of children in the US have elevated blood lead concentrations, many of them are asymptomatic.14 The primary concern in this group is that multiple meta-analyses have demonstrated that, even at low blood lead concentrations, there is an inverse relationship between blood lead concentrations and intelligence quotient scores as well as markers of academic achievement. Furthermore, some research suggests that the dose-response curve is steeper at lower blood lead concentrations, meaning that the number of IQ points lost per unit increase in blood lead concentration is higher in the 1 to 10 mcg/dL lead range than in the 10 to 20 mcg/dL range.14
Emerging Research
Recent reporting suggests that the regular consumption of beverages in glazed, ceramic cups may increase the chances of lead-related health risks.15,16 In one study, the chronic daily intake of lead by children and adults consuming from new ceramic cups was 1.3-5 times and 1.28-6 times more than that from old ceramic cups.15 The intake values far exceeded the WHO reference dose of 0.0006 mg Pb/kg bw/day in children (<11 years) and 0.0013 mg Pb/kg bw/day in adults. According to the study, these levels of lead consumption in children might be predicted to be associated with a decrement in IQ by at least one point and associated with adverse effects in adults, especially in women of childbearing age.15
Studies suggest a significant association between lead exposure and mortality from all causes, cardiovascular disease, and cancer in general populations.17 Specific to cancer, epidemiological evidence continues to illustrate a link between blood lead concentration and death rate due to cancer in a number of populations, including in the US,18 South Korea,19 and Australia.20 In June 2018, the first study to demonstrate urinary lead concentration as an independent predictor of cancer mortality in the general population was published in Frontiers in Oncology.2 Using National Health and Nutrition Examination Survey 1999-2010 data and its Mortality Follow-Up study, Li et al found that lead exposure continues to be a significant determinant of cancer mortality in the US, despite decreased amounts of environmental lead levels, and that monitoring urinary lead levels is a non-invasive approach that may support biomarker discovery and clinical research.2
Conclusion
While the concept that toxic chemicals accumulate in the body and are the cause of various health problems has long been a fundamental tenet of traditional healthcare systems around the world, researchers have learned a great deal in recent years about how toxins and toxicants affect us, where they originate, and how to improve our ability to detoxify in a toxic world. Understanding toxicity and taking practical steps to improve biotransformation are essential parts of any integrative approach to your patients’ health and well-being.
The most important aspect of management in a patient with an elevated blood lead concentration is identifying the source of lead and removing it from the patient’s environment if possible.14 Optimizing the patient’s nutritional status is also paramount, with particular attention to ensuring adequate nutrient intake, including iron and calcium.21-23 What other steps can clinicians take to recognize toxicity in their patients? Learn more at IFM’s Environmental Health Advanced Practice Module (APM).
Related Articles
Detoxification: Supporting Liver Function With Nutrition
Healthy Food Preparation: Reducing Toxicant Exposures
References
- Liu X, Wu J, Shi W, Shi W, Liu H, Wu X. Lead induces genotoxicity via oxidative stress and promoter methylation of DNA repair genes in human lymphoblastoid TK6 cells. Med Sci Monit. 2018;24:4295-4304. doi:12659/MSM.908425
- Li S, Wang J, Zhang B, et al. Urinary lead concentration is an independent predictor of cancer mortality in the US general population. Front Oncol. 2018;8:242. doi:3389/fonc.2018.00242
- Lead poisoning. World Health Organization. Published August 31, 2022. Accessed July 19, 2023. https://www.who.int/news-room/fact-sheets/detail/lead-poisoning-and-health
- Rana MN, Tangpong J, Rahman MM. Toxicodynamics of lead, cadmium, mercury and arsenic-induced kidney toxicity and treatment strategy: a mini review. Toxicol Rep. 2018;5:704-713. doi:1016/j.toxrep.2018.05.012
- Nagaraju R, Kalahasthi R, Balachandar R, Bagepally BS. Association between lead exposure and DNA damage (genotoxicity): systematic review and meta-analysis. Arch Toxicol. 2022;96(11):2899-2911. doi:1007/s00204-022-03352-9
- Lanphear BP, Rauch S, Auinger P, Allen RW, Hornung RW. Low-level lead exposure and mortality in US adults: a population-based cohort study. Lancet Public Health. 2018;3(4):E177-E184. doi:1016/S2468-2667(18)30025-2
- Obeng-Gyasi E. Lead exposure and cardiovascular disease among young and middle-aged adults. Med Sci (Basel). 2019;7(11):E103. doi:3390/medsci7110103
- Agency for Toxic Substances and Disease Registry. Lead toxicity: what are possible health effects from lead exposure? Centers for Disease Control and Prevention. Reviewed May 24, 2023. Accessed July 19, 2023. https://www.atsdr.cdc.gov/csem/leadtoxicity/physiological_effects.html
- He L, Chen Z, Dai B, Li G, Zhu G. Low-level lead exposure and cardiovascular disease: the roles of telomere shortening and lipid disturbance. J Toxicol Sci. 2018;43(11):623-630. doi:2131/jts.43.623
- Jalili C, Kazemi M, Cheng H, et al. Associations between exposure to heavy metals and the risk of chronic kidney disease: a systematic review and meta-analysis. Crit Rev Toxicol. 2021;51(2):165-182. doi:1080/10408444.2021.1891196
- Boskabady M, Marefati N, Farkhondeh T, Shakeri F, Farshbaf A, Boskabady MH. The effect of environmental lead exposure on human health and the contribution of inflammatory mechanisms, a review. Environ Int. 2018;120:404-420. doi:1016/j.envint.2018.08.013
- National Center for Environmental Health, Division of Environmental Health Science and Practice. Childhood lead poisoning prevention: CDC updates blood lead reference value to 5 µg/dL. Centers for Disease Control and Prevention. Reviewed December 16, 2022. Accessed July 19, 2023. https://www.cdc.gov/nceh/lead/news/cdc-updates-blood-lead-reference-value.html
- Reuben A, Schaefer JD, Moffitt TE, et al. Association of childhood lead exposure with adult personality traits and lifelong mental health. JAMA Psychiatry. 2019;76(4):418-425. doi:1001/jamapsychiatry.2018.4192
- Halmo L, Nappe TM. Lead Toxicity. StatPearls; July 4, 2022. Accessed July 19, 2023. https://www.ncbi.nlm.nih.gov/books/NBK541097/
- Mandal PR, Das S. Leachable lead and cadmium in microwave-heated ceramic cups: possible health hazard to human. Environ Sci Pollut Res Int. 2018;25(29):28954-28960. doi:1007/s11356-018-2944-8
- Hore P, Alex-Oni K, Bardhi N, Sedlar S. Notes from the field: lead poisoning in a family of five resulting from use of traditional glazed ceramic ware – New York City, 2017-2022. MMWR Morb Mortal Wkly Rep. 2022;71(22):743-744. doi:15585/mmwr.mm7122a3
- Guo X, Su W, Li N, et al. Association of urinary or blood heavy metals and mortality from all causes, cardiovascular disease, and cancer in the general population: a systematic review and meta-analysis of cohort studies. Environ Sci Pollut Res Int. 2022;29(45):67483-67503. doi:1007/s11356-022-22353-w
- Cheung MR. Blood lead concentration correlates with all cause, all cancer and lung cancer mortality in adults: a population-based study. Asian Pac J Cancer Prev. 2013;14(5):3105-3108. doi:7314/APJCP.2013.14.5.3105
- Kim M-G, Ryoo J-H, Chang S-J, et al. Blood lead levels and cause-specific mortality of inorganic lead-exposed workers in South Korea. PLoS One. 2015;10(10):E140360. doi:1371/journal.pone.0140360
- Gwini S, MacFarlane E, Del Monaco A, et al. Cancer incidence, mortality, and blood lead levels among workers exposed to inorganic lead. Ann Epidemiol. 2012;22(4):270-276. doi:1016/j.annepidem.2012.01.003
- WIC Works Resource System. Protect against lead exposure with WIC foods. USDA. Accessed July 20, 2023. https://wicworks.fns.usda.gov/resources/protect-against-lead-exposure-wic-foods
- McElroy KG, Iobst SE, DeVance-Wilson C, Ludeman E, Barr E. Systematic review and meta-analysis of the effect of nutrients on blood lead levels in pregnancy. J Obstet Gynecol Neonatal Nurs. 2020;49(3):243-253. doi:1016/j.jogn.2020.02.004
- Upadhyay K, Viramgami A, Bagepally BS, Balachandar R. Association between blood lead levels and markers of calcium homeostasis: a systematic review and meta-analysis. Sci Rep. 2022;12(1):1850. doi:1038/s41598-022-05976-4